Overactive Bladder
Overactive bladder symptoms
Overactive bladder (OAB) refers to a group of symptoms that may occur alone, or more commonly, in combination with one another symptom. These include:
- Urinary frequency – You have to go to bathroom too often to pass urine.
- Urinary urgency – You have to rush to the bathroom urinate.
- Nocturia – You wake up at night to urinate.
- Urge incontinence – You rush to the bathroom, but you don’t get there in time and leak urine.
Is overactive bladder serious?
Overactive bladder is very rarely serious and has many different causes. Most commonly, it is just very annoying and bothersome because a person spends so much time in the bathroom and/or trying to figure out where the next bathroom is. Many people with overactive bladder limit their activities because they are embarrassed by going so often or fearful that they won’t get to the bathroom in time.
What causes of overactive bladder in women?
There are many different causes. The most common causes are listed here.
- Cystitis – You have a bladder infection.
- Polyuria (poly =many, uria = urine) – Your kidneys make too much urine.
- Pelvic organ prolapse – You have a” dropped bladder” which is kind of like a hernia. You feel a bulge or heaviness in the vagina because the bladder (or sometimes the uterus or rectum) has dropped.
- Urethral obstruction – Your flow of urine is blocked, like a kink in a garden hose or a clogged pipe.
- Idiopathic – You have symptoms of overactive bladder, but doctors don’t know what is causing it.
The good news is that, in most instances, when the cause is treated, the overactive bladder symptoms go away.
How is overactive bladder is treated?
Most doctors treat OAB empirically. That means that based on their experience, they treat you by trial and error without first determining the actual cause of your symptoms. They usually start with the least invasive treatments, such as educating you on how you can change your behavior to lessen your symptoms (called “behavior modification”) and/or prescribing a medication. Only when these treatments fail, do they go on to a more sophisticated evaluation to find the underlying cause. This is the way that most medical organizations recommend that patients be treated, because from a practical and economic standpoint, it makes sense. It ensures that the largest number of patients can get treated in a timely fashion. We call that a “top-down approach” because it treats the majority of women the same way. You only get treatment tailored to your specific needs, if you don’t get better. Sadly, too many patients don’t get better using this approach, and even if they do, it takes much longer than necessary. The WeShare app and software platform offers the possibility of a different approach to diagnosis treatment that we call the “bottom-up approach.” With this method, you and your doctor can begin (and sometimes complete) the evaluation necessary to determine the actual cause of your symptoms before you even come into the office, so you are one step closer to feeling better. When you actually see your doctor face-to-face, you can discuss whether the treatment is working or if it needs to be changed. Sometimes, you don’t even need to go into the office to get better. The entire process of diagnosis and treatment can be completed with telemedicine visits. A telemedicine visit is completed remotely by telephone, video, secure email or through a web-based portal. This likely makes sense to you now that the COVID crisis has made going to the physician’s office less desireable.
What are the treatments?
First, you and your doctor will search for and treat any remediable conditions. Remediable conditions are those whose treatment cures or improves the overactive bladder symptoms. For example, polyuria (your kidneys make too much urine) is a remedial condition. If the polyuria is caused by diabetes, you treat the diabetes and the polyuria gets better and so do the overactive bladder symptoms.
If you do not have are mediable condition, treatment is aimed at addressing the symptoms using combinations of lifestyle and behavioral approaches, medications, neuromodulation and surgeries. The particulars of these treatments will be the focus of another segment.
Example of a telemedicine visit using the weShare URO® app
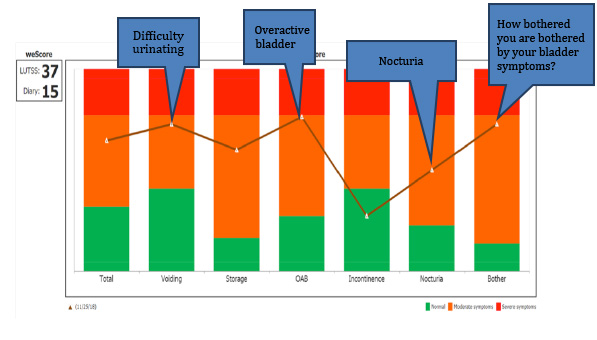
A 49-year-old, healthy woman contacted her doctor’s office because she had overactive bladder symptoms (see above for the definition of OAB). She was asked to download the weShare URO® app which includes a questionnaire about her symptoms and a bladder diary in which she records her symptoms for 24 hours. Here is the result of a questionnaire:
Lower Urinary Tract Symptoms (LUTS)
Urinary frequency
There are no exact normal numbers, although most people urinate about 6 – 8 times a day. When we ask patients how often they normally urinate, the most common answer is, “it varies.” Of course, “it varies.” Everything varies.
This is a graph showing her symptoms. The higher the point is on the graph the worse the symptoms. Red indicates the worst possible symptoms and green indicates little or no symptoms. This woman has severe voiding, OAB and nocturia symptoms and, she is bothered a lot by her symptoms.
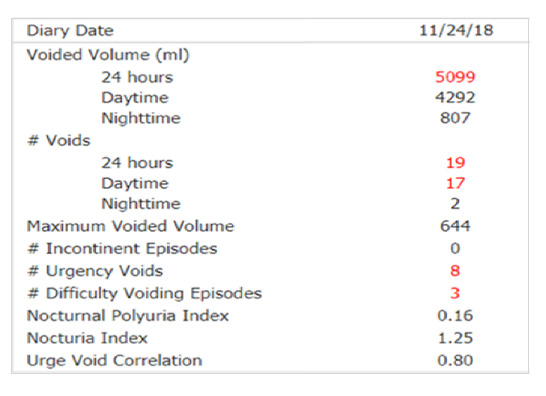
Here are the results of her bladder diary:
The numbers highlighted in red are abnormal. Voided volume is the total amount of urine and that she urinated in 24 hours – 5099 mL – over 5 liters, that’s 1.3 gallons, more than twice what is normal! # voids is how many times she urinated in 24 hours -19 times, also more than twice normal and she had to rush to the bathroom 8 times and had difficulty urinating 3 times. These are terrible symptoms, all caused by polyuria – making too much urine.
The first step in treatment was to make sure she did not have a more serious condition. An example is diabetes which would make her drink too much, because the more you drink, the more urine your kidneys make. She did not have a more serious condition. Instead of coming into the office, she and her doctor agreed to do a telemedicine visit. During the visit, her doctor confirmed that it was ok for her to cut back on how much she drinks. She was able to cut back on how much liquid she drank by about 50%. Remarkably, all of her symptoms got better, and she never had to come into the office!
Download Brochure